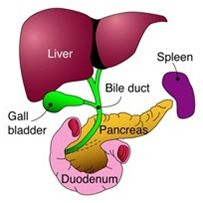
The pancreas is a gland that lies towards the back of the upper part of the abdomen. It is divided into head, neck, body and tail. Pancreatic juice emptied into duodenum through pancreatic duct at a point where bile duct joins pancreatic duct.The Pancreas
The two main functions of pancreas is secretion of insulin to control blood sugar and makes enzymes which help in digestion of fat.
Acute Pancreatitis
It is an acute inflammation of the pancreas,where the pancreas becomes swollen and leaks its juices.Acute Pancreatitis may be mild, moderate or severe.
Most of the patient develop mild pancreatitis(80%). Mild pancreatitis is a self remitting disease and most of the patients are better within few days with supportive treatment though they require hospitalization.
Moderate and severe type of pancreatitis take long time for recovery sometime may upto months. Those patients who develop complications related to pancreatitis need to be managed in specialized centre. Even in best of the centres around the world, severe pancreatitis patient can succumb to it.
Common Causes:
- Gallstones
- Alcohol excess
- Idiopathic (i.e. the cause is unclear)
- Some rarer causes are:
- Certain viral infections such as Mumps and Coxsackie B
- Trauma
- Post major surgery
- After ERCP (an endoscopic procedure)
- Pancreatic cancer
- Certain drugs (azathioprine, , steroids)
- Hyperparathyoidism
- Hypertriglyceridemia
- Pancreas divisum
Symptoms
- Severe abdominal pain
- Vomiting
- Jaundice
- fever
- abdominal distension
Diagnosis
Based on the typical history of upper abdominal pain radiating to the back the diagnosis of acute pancreatitis is suspected. Presence of high blood amylase or lipase or imaging (ultrasound/CT/MRI) will clinch the diagnosis. All tests are not required to diagnose acute pancreatitis, presence of two of the three things ( history, amylase/lipase or imaging) is enough to diagnose this condition.
Treatment
Any patient diagnosed to have acute pancreatitis should be treated in a specalist center experienced in managing these cases. These patients are initially admitted in intensive care for monitoring and treatment. Initial treatment consists of intravenous fluid administration, painkillers and sometimes oxygen support. Mild acute pancreatitis usually resolves with these simple measures within a week. Patients are monitored for pulse, blood pressure, urine output, blood oxygen levels in the ICU. If they improve they are shifted to the ward in cases of mild attacks.
Some patients develop more severe form of pancreatitis and requires prolonged ICU stay. Their pancreas may become necrotic or dead, partly or wholly and may get infected. They may develop collection of fluid, pus or necrotic material inside abdomen. Some patients may develop organ failure (kidney, heart or respiratory failure).
Ultrasound and liver function test are always done initially to rule out gallbladder stone as the cause of pancreatitis. If gallbladder stone is found to be blocking bile duct or causing fever with chills it needs to be cleared with ERCP (Endoscopic Retrograde Cholangiopancreatography); an endoscopic method of bile duct stone removal.
Treatment is like mild cases, but may continue for a longer duration. When they develop infection antibiotics may be required to treat that. This usually ocuurs in the 3rd or 4th week of disease. Clear fluid collections (acute peripancreatic fluid collection) in the early stages of the disease usually resolves spontaneously and do not require any drainage. When they develop wall around the collection (Pseudocyst) they may be left alone if asymptomatic or may be drained internally by endoscopic or laparoscopic/open surgical method if they develop pain abdomen or vomiting.
When the pancreas is necrotic, initially these patients will develop acute necrotic collection and later on walled off pancreatic necrosis. These will require some form of drainage if they are not improving with medical treatment. Drainage is initially by percutaneous means, if this technique fails surgical removal (necrosectomy) is necessary. Surgery gives best result if it is done after 4 weeks.
In all cases of acute pancreatitis patients are allowed normal diet as soon as possible , otherwise a tube is placed in the stomach or jejunum and fed through that.
Where there is organ failure, ventilator support for lungs or dialysis for kidney may be required.
Contrast enhanced CT or MRI may be required in severe cases to confirm necrosis and to plan interventions (percutaneous or surgical drainage). This may need to be repeated depending the clinical course of the patient.
What causes chronic pancreatitis?
There are several causes of chronic pancreatitis. The main causes are following:
- Excess alcohol intake is the commonest cause .
- Idiopathic
- Tropical pancreatitis
- Hypercalcemia
- Hypertriglyceridemia
- Hereditary
- Repeated attack of acute pancreatitis
- Pancreatic duct stricture/Congenital abnormality (pancreatic divisum)
- Autoimmune pancreatitis
Symptoms
- Pain is the most disabling symptom.
- Diabetes , about 30% of the chronic pancreatitis patient develop diabetes.
- Loose , greasy stool
- Jaundice, if it invoives the lower end of the bile duct.
- Weight loss can occur
- Compression of the duodenum can lead to vomiting
- Bleeding into the gut can sometimes be the first symptom
Test
- Blood test to see if you have already develop diabetes or not.
Pancreatic enzyme assessment is not rotuiely done in clinical practice. - CT scan/MRCP is done to look at the pancreatic structural changes and diagnose chronic pancreatitis.
- EUS( endo ultrasound) some is done to diagnose chronic pancreatitis.
Treatment
All patient of chronic pancreatitis need to undersand problems arising due to the disease can be managed medically or surgically though there is no cure for the disease at present.
- Pain relief: all patient are given pain killers initially to control the pain but if it still continue to affect them, surgical intervention can cure pain upto 90% of the patient.
- Diabetes : medical management
- Pancreatic enzyme deficiency: Pancreatic enzymes to be taken at the time of meals
- Surgical procedures: These are indicated in following condition
- Intractable pain
- Pancreatic duct stenosis (narrowing)
- Cysts and pseudocysts
- Biliary obstruction
- Duodenal obstruction
- Suspicion of cancer
- Portal or splenic vein thrombosis
Pancreatic tumours can be adenocarcinoma, cystic neoplasms or endocrine tumours. Adenocarcinoma is the commonest and pancreas cancer is synonymous with it. In general, cystic neoplasms and endocrine tumours have better outcome than adenocarcinoma.
It is common in older people, with a peak incidence in the 65-75 years age-group. It is slightly more common in males. Tobacco smoking increases the risk.Certain genetic factors and medical conditions can increase the risk of developing pancreatic cancer.
Symptoms
Most of the pancreatic cancer when detected are at an advanced stage. The common symptom are :
- Obstructive jaundice i.e. yellow colour of the eyes and skin, itching of the skin, and passing dark urine
- Weight loss with back pain
- Recent-onset diabetes mellitus
- Unexplained attack of pancreatitis
What tests are done to diagnose pancreatic cancer?
- LFT- to ascertain jaundice and level of jaundice
- Tumour marker CA19-9, raised level of tumour marker is suggestive of tumour though not confirmatory.
- Ultra sound abdomen is the intial scan which gives an idea about the tumour site.
- Triphasic CT scan Abomen- Show the site of the tumour, its local spread, involvement of the vasculature.
- MRI is another useful scan that yields information similar to CT, but also gives three-dimensional reconstruction of the bile ducts (called MRCP). This can provide a roadmap for the biliary anatomy above and below the tumour.
- PET scanning can detect pancreatic cancer well as the presence of distant spread, but its use is not routine.
- EUS (endoscopic ultrasound) increasingly plays a role in the diagnosis of pancreatic cancer and can also guide fine needle aspiration of a cell sample.
Treatment
For the majority of patients with pancreatic cancer, by the time they develop symptoms and the diagnosis is made, their disease is too advanced to be cured by surgery.
If scans shows that the tumour is potentially operable, then the patient should be considered for surgical resection, as that offers a chance of a cure. Tumours of the ampulla have a good prognosis and should, if at all possible, be resected. Some of the rare tumours and the neuroendocrine lesions should also be resected if at all possible.
For those patients who have inoperable disease, palliative treatments are offered. These include chemotherapy and radiation (or occasionally both), and measures to relieve symptoms
Surgical resection
The standard resection for a tumour of the pancreatic head or the ampulla is a Pancreatoduodenectomy. Originally known as the Whipple operation, this involves removal of the pancreatic head, along with the duodenum and the lower part of the bile duct.
Resectional surgery for pancreatic cancer should be carried out in specialist units. There is a clear correlation between higher caseload volume and lower hospital mortality and morbidity. The operation should carry a mortality rate of no more than 3-5%. But around a third of patients develop a complication in the postoperative period.
These complications are usually infective, but a leak from the anastomosis between the pancreas and the bowel is known to occur in at least 10% of patients, and this can give rise to major complications. Mean in-patient stays range from 12 to 16 days.
Adjuvant treatment after surgery
With surgery alone, the 5-year survival following resection of a pancreatic adenocarcinoma ranges around 10-20%, and figures of upto 25% have been reported. Patients with resected ampullary tumours have 5-year survivals of 40-50%, and cystic tumours and neuroendocrine tumours can often be cured by surgical resection.
Palliation
If inoperable disease is found in the course of an operation that was commenced with the intent to remove the tumour, a choledocho-enterostomy (diversion of the bile flow into the gut) and a gastro-enterostomy (diversion of the flow of food, bypassing the duodenum) can be carried out, to relieve jaundice and duodenal obstruction.
In patients found to have unresectable disease on scans, jaundice is relieved by stenting at ERCP. Plastic stents tend to block faster, and if the patient is likely to have a longer life-expectancy, a self-expanding mesh metal stent can be used. If the patient is not a suitable candidate for endoscopic stenting, a percutaneous transhepatic stent can be placed. This involves puncturing the skin and placing a stent through the liver substance, and is done in the X-ray department.
Obstruction of the duodenum occurs in approximately 15% of cases; if this occurs early in the course of the disease, surgical bypass by gastrojejunostomy is appropriate, but if it is late in the course of the disease then the use of expanding metal stents inserted endoscopically should be considered.
If no operative procedure is undertaken, biopsy of the tumour should be performed before consideration of chemotherapy or chemoradiation. The role of chemotherapy in the management of pancreatic cancer remains ill-defined. For the patients with ductal adenocarcinoma, 5-FU or gemcitabine will produce a remission in 15-25% of patients. No long-term cures have been described with chemotherapy or radiotherapy.
Whipples operation
It is also occasionally referred to as a pancreaticduodenectomy in reference to the organs that are removed. During the Whipple’s operation, the head of pancreas, a portion of the bile duct, the gallbladder and the duodenum are removed, usually with part of the stomach.
After removal of these structures, the remaining pancreas, bile duct and stomach are rejoined to the intestine. This allows pancreatic juice, bile and food to flow back into the gut, so that digestion can proceed normally. The operation normally lasts four to seven hours.
Benefit of surgery
The aim of surgery is to remove all of the visible tumour.
This means that you should live longer, with a better quality of life than you would without the operation. Without surgery, the average survival of patients with pancreatic cancer is less than one year. Your survival length should be longer if you are having the Whipple’s operation for a non-cancerous condition. A successful Whipple’s operation can improve your chance of survival at two years to 40-60%, and survival at five years is 20-30%. With other types of tumours, the results are often better.
Although you will need time to recover from the operation, almost all
patients who have this surgery get back to living their normal life. You should be able to eat and drink normally (although you will be given enzyme supplements to help your digestion) and get back to all your usual activities.
Post operative
- You will have to stay in surgical itu for 1-2 days.
- you will have many tubes attached to your body that you didn’t have before going to theatre.
- You may find these frightening and uncomfortable but as your condition improves they will decrease in number.
- It is normal to have some or all of these after this kind of surgery:
- tubes resting on your nostrils or a plastic mask attached to a thick tube
- to give you oxygen
- a tube in your nose to provide liquid feed down into your tummy while
- the joins heal
- a tube in your nose to collect excess acid and bile from your stomach
- a tube stuck to your neck with a clear plaster for drips, medication, and
- monitoring blood flow and sometimes to give special liquid food
- drips in your arms/hands to keep you hydrated
- thick tubes called drains to collect excess fluid from the operation site
- sometimes a feeding tube into your tummy
- dressings over the wound site (1st 48 hours) then either underneath
- this the wound may have blue stitches, or surgical clips, or it
- may have been closed with invisible absorbable stitches.
- a catheter (tube into your bladder to collect urine).
Most of these tubes and drains are removed by the end of your first week in hospital, occasionally you will still have a tube coming out of your tummy when you first go home. If this is necessary then we will make sure that you understand why it is there and know how to look after it until we remove it in clinic.
The length of stay in hospital after this surgery is quite variable, but the average is ten to 14 days. If you are over 75 or have other health problems you may need to stay in longer, whilst some very fit patients may go home as early as one week after the operation if they recover quickly. If you have complications after this surgery occasionally you need to stay in much longer.
Possible risk and complications
Most complications are minor and just slow down your recovery a little, however some are much more serious and may mean you stay in hospital for a lot longer than you expected. Possible complications include:
- General anaesthetic complications: these have been minimised by improvements in pre-operative evaluation and peri-operative care, however major surgery such as this places a huge strain on the body’s resources; the risks for any individual patient are different and are assessed person by person. If we think the risks are too great then we will advise against surgery.
- Chest infection and problems with breathing
- Bleeding during the operation, which may result in blood transfusion
- Wound infection
- Blood clots forming in the legs
- Anastomotic leak: During the operation the surgeon will join together the pancreas, stomach, small bowel and bile duct. Occasionally, one of these joins can leak after the operation. The join that is most likely to leak is that between the pancreas and bowel , this join is most likely to leak because of the caustic nature of the substances passing through it. Pancreatic juice contains very potent digestive enzymes, which can break down proteins trying to heal the join and thus disrupt the econstruction. If you have a leak then some of the plastic drain tubes coming out of your tummy will be left in place to drain the fluid off until the leak has stopped. Rarely a leak can damage blood vessels close to the pancreas and can cause serious bleeding several days after your operation, this is the most serious complication after this type of surgery and often requires an operation to repair the blood vessel.
- Delayed emptying of the stomach: After the surgery, some patients take longer to get back to normal eating and drinking because of slow recovery of the normal actions of the stomach. This is called delayed gastric emptying. During this time, if it happens to you, you will have a drip going into your vein to keep you hydrated with fluids. You will also be fed with liquid food, which will pass into your body through a tube until your stomach has recovered enough to take in food through your mouth. Some patients take a little while longer to recover and may need to continue with tube feeds for several weeks.